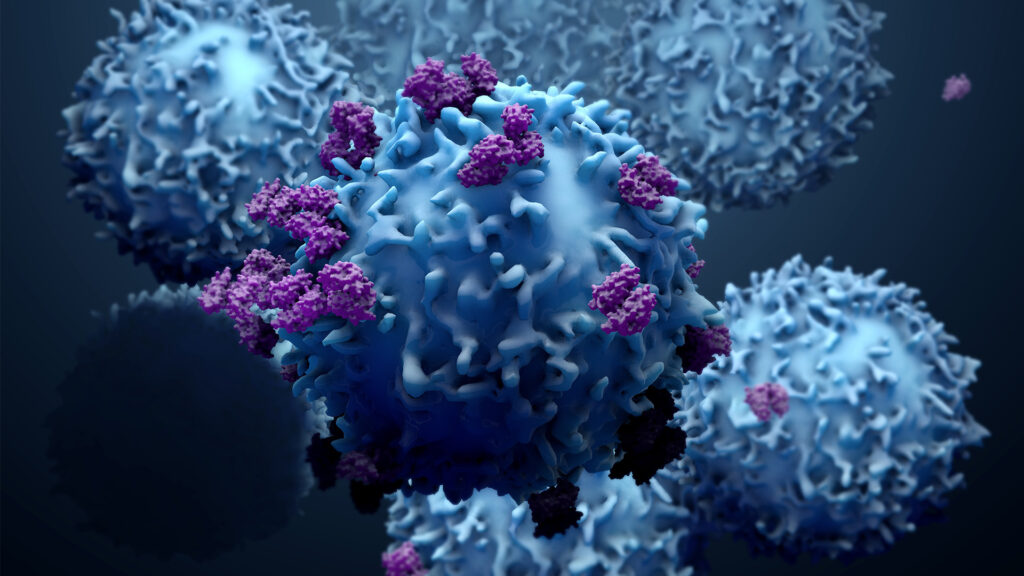
SRI scientists are developing a cell-based platform using an often-undervalued subset of helper T cells to deliver potent antitumor proteins for solid tumors, overcoming dose-related toxicities.
Today’s drug delivery platforms rely on synthetic carriers, which overlook patient variability. Result: They can often harm healthy tissues. What’s more, these medicines are often limited in availability, and because they have short half-lives, they often require multiple doses.
Against that backdrop, a new paper released in the Proceedings of the National Academy of Sciences (PNAS) describes how SRI researchers have transformed an overlooked helper CD4 T cell into a cell-based platform for delivering desired therapeutic proteins.
For nearly a decade, initially supported by the NIH Director’s New Innovator Award and multiple grants from the National Cancer Institute’s Innovative Molecular Analysis Technologies (IMAT) Program, Parijat Bhatnagar, Senior Program Director of Cell-based Medicine at SRI and senior author of the paper, has been leading a cross-disciplinary team of scientists to develop this breakthrough precision medicine technology.
Finding a direct pathway to a cure
“Most T cell therapies focus on CD8 killer T cells, which can destroy cancer cells that over-express cancer-associated biomarkers, which is where we initially focused,” says team member Harikrishnan Radhakrishnan, lead author of the paper. “We discovered that while our process was designed to generate CD8 killer T cells as a delivery system, the pathway we aimed to harness for in situ protein production was far more active in the helper CD4 T cells,” he explains.
The team first developed a process for engineering and expanding primary T cells. They applied this process to create three CD4 and CD8 T cell types, each with a distinct intracellular domain of the chimeric antigen receptors (CAR). They studied their ability to deliver desired proteins to the tumor cells. Findings revealed that CD4 T cells engineered with a CAR containing the 4-1BB intracellular domain, not CD28, were the most effective in mobilizing the pathway for delivery — outperforming CD8 T cells. In fact, including the CD28 domain alongside 4-1BB reduced the delivery function in both CD4 and CD8 T cells.
“A cell that assembles medicine exactly where and when it’s needed, in proportion to the tumor size and without harming healthy tissues, fascinates me.” — Parijat Bhatnagar
“Because CD4 T cells remain in the body for decades and modulate their response to stimuli, we anticipate that our delivery platform will be able to synthesize therapeutic proteins specifically at disease sites, in proportion to the disease burden, without impacting healthy tissues, and sustain for extended periods,” says Bhatnagar.
Targeting ovarian cancer cells
The team directed the platform to express interferon-beta (IFNβ), a therapeutic protein with strong antitumor effects that can be lethal if delivered in excess, for specifically targeting ovarian cancer. The results were striking — IFNβ delivered through CD4 T cells, when stimulated by cancer cells, proved significantly more effective in controlling the tumor compared to much higher amounts of directly injected IFNβ. Bhatnagar is now extending his studies to better understand the platform and adapting it to other cancers and, possibly, other diseases.
“A cell that assembles medicine exactly where and when it’s needed, in proportion to the tumor size and without harming healthy tissues, fascinates me. I look forward to seeing it used in clinical settings,” says Bhatnagar.
Learn more about our innovations in health.
This research was supported in part by the National Institute of Biomedical Imaging and Bioengineering (DP2EB024245: NIH Director’s New Innovator Award Program; the National Cancer Institute (R21CA236640, R33CA247739, R21CA288900, R61CA281785) of the National Institutes of Health (NIH); and the Defense Advanced Research Projects Agency (DARPA) (D19AP00024: DARPA Young Faculty Award.