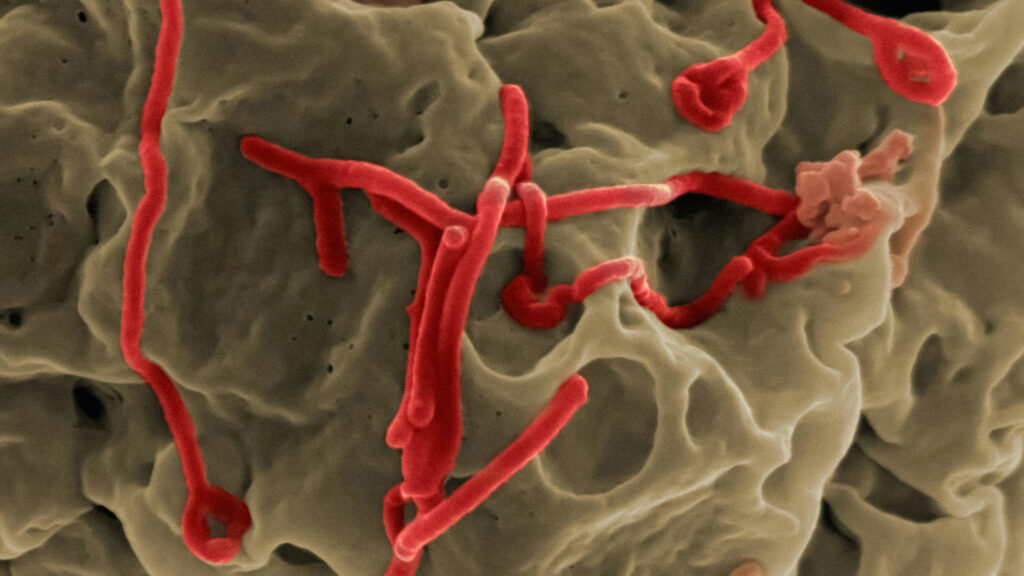
Machine learning algorithms identify how hemorrhagic fever viruses hijack human cells.
Hemorrhagic fever viruses, such as Ebola and Yellow fever, have devastating impacts on both people and the animals they depend on. Researchers at SRI, in collaboration with teams at Virginia Tech and the University of Montreal, are using AI to find new ways to understand and fight potentially deadly viruses.
In a recent paper, the researchers identified a host’s antiviral immune response to the Rift Valley fever virus (RVFV), a hemorrhagic virus found primarily in sub-Saharan Africa. This is the first step in developing therapeutics to fight RVFV and potentially other hemorrhagic fever viruses that attack the immune system in similar ways. The AI tools they’ve developed helped identify other ways in which hemorrhagic fever viruses hijack cells, providing potential targets for drug development down the line.
“We’re integrating AI with our work in biology in order to characterize hemorrhagic fever viruses and determine how they manipulate their hosts,” said Paul O’Maille, Program Director of Biocomplexity Sciences at SRI. “Our research will potentially lead to the development of new drugs that can stop these viruses in their tracks.”
RVFV, which currently has no FDA-approved vaccines or treatments, can infect people and livestock. In people, symptoms of the mosquito-borne virus are usually mild, but severe cases can cause liver disease, brain swelling, and hemorrhagic fever. In livestock, the virus is more deadly. It is almost always fatal for young cows, sheep, and goats, and it kills about 30% of adult livestock that catch it. Additionally, it causes almost 100% of pregnant livestock to miscarry.
“The computational AI allows us to look at vast numbers of sequences to determine realistic interactions.” — Paul O’Maille
“It’s an important virus to learn more about — it has a significant economic and public health impact,” said Kylene Kehn-Hall, a professor of virology at Virginia Tech and the principal investigator on the project.
To understand how RVFV interacts with a host’s cells, the researchers are looking at short linear motifs (SLiMs), which are short sequences of amino acids that bind to proteins and coordinate the cellular process. Viruses have evolved to mimic host SLiMs to gain control over the host’s natural process, forcing infected host cells to act in ways that help the virus spread. There are many potential SLiMs and many potential binding sites — identifying even a single viral SLiM, finding where it interacts with the host, and determining if blocking that interaction would stop the virus can take years using experimental methods alone.
AI dramatically speeds up the process. Researchers at SRI have developed a predictive model trained on databases of known SLiM sequences and their host interactions to generate and identify SLiMs in hemorrhagic fever viruses that could interfere with and control host cells. The SLiMs are reviewed by biochemists and shared with virologists, who conduct experiments to test and understand interactions in cells.
“The computational AI allows us to look at vast numbers of sequences and conduct biophysical simulations to determine realistic SLiM interactions,” O’Maille said. “Our collaborators can zero in on the cell biology and validate the findings to unravel how hemorrhagic fever viruses work.”
The results are fed back into the machine learning algorithm, helping to improve the AI’s predictions. The results are carried forward, making it easier to learn about other hemorrhagic fever viruses, even if they’re not using the same SLiMs, since many viruses rely on the same tricks to spread in the body.
“SRI is bringing our unique multidisciplinary approach to tackle complex, real-world problems in the field of computational biology,” said O’Maille.
Learn more about our innovations in artificial intelligence and health.